Cystic fibrosis (CF) is one of the most common fatal genetic disorders worldwide, affecting approximately 100,000 individuals. People with CF suffer from chronic lung infections and have a reduced life expectancy [1]. The disease is caused by specific changes (‘variants’) in a gene called the CF transmembrane conductance regulator (CFTR).
CFTR is found mainly on epithelial cells, which coat the lining of the lungs, and it is necessary for normal lung function. The mutated form of CFTR made in CF patients causes mucous to accumulate in their lungs, which allows bacteria to colonise and establish persistent infections [2].
The most common bacterial pathogen infecting CF patients is called Pseudomonas aeruginosa, a species that happily lives in the environment just as well as in human lungs. Last year, we published the largest study of Pseudomonas to date [3], and we found evidence that it is adapting to specifically infect humans.
In recent years, a new class of drugs called modulators has transformed CF treatment. These drugs substantially improve patient quality of life, by increasing CFTR activity, but they do not eradicate bacteria from the lungs. This means that Pseudomonas infections continue to cause inflammation and damage [4]. Understanding how and why the bacteria persist is important for the development of new treatments.
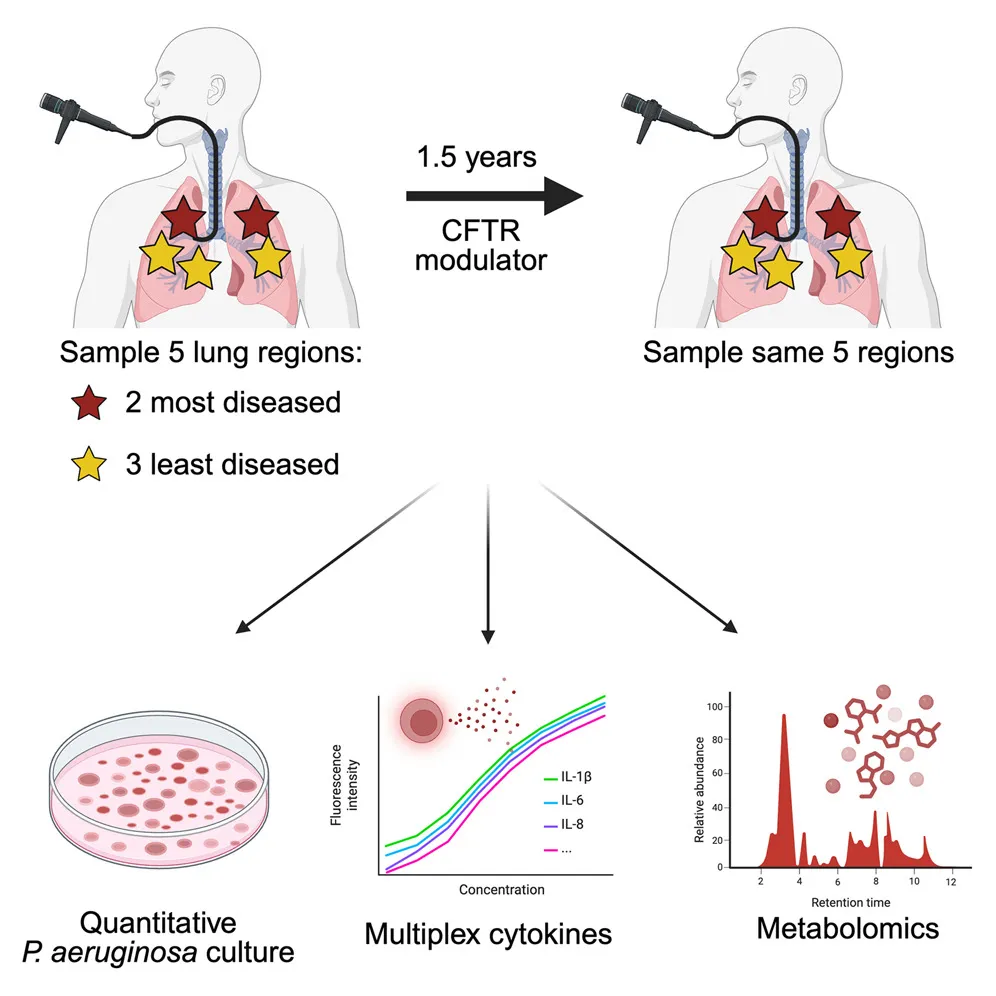
A recent paper in the journal Cell Host & Microbe [5] investigated the extent of lung infections pre- and post-treatment with modulator drugs. They found an all-or-nothing response to modulator treatment: either the bacteria was completely eradicated, or it remained widespread throughout the lungs. Inflammation was especially driven by Pseudomonas infections, which are capable of surviving treatment.
The authors speculate that bacteria in different regions of the lungs are genetically adapted to local conditions, allowing them to persist. This raises the intriguing possibility that the adaptations responsible are mediated via gene regulatory networks that allow the bacteria to grow in different parts of the body.
References
- https://jamanetwork.com/journals/jama/article-abstract/2805701
- https://www.nature.com/articles/s41572-024-00538-6
- https://www.science.org/doi/10.1126/science.adi0908
- https://www.cysticfibrosisjournal.com/article/S1569-1993(23)01669-7/fulltext
- https://www.cell.com/cell-host-microbe/fulltext/S1931-3128(25)00281-